Bio-printing: Advancements in Organ Regeneration in Regenerative Biomedicine
Recent advancements in the field of regenerative biomedicine have revolutionized organ regeneration through a cutting-edge technology known as bio-printing. This innovative approach allows for the precise fabrication of functional tissues and organs using three-dimensional (3D) printing techniques coupled with cell-based strategies. One compelling example is the successful transplantation of a 3D printed kidney into a patient suffering from end-stage renal disease, which not only restored their renal function but also significantly improved their quality of life.
Bio-printing involves the layer-by-layer deposition of cells, biomaterials, and growth factors to construct complex tissue structures that mimic native physiology. By precisely positioning each cell type within the desired architecture, this technique enables researchers to recreate intricate tissue microenvironments while ensuring proper functionality. Moreover, bio-printing offers potential solutions to address organ shortages by providing an alternative source for transplantable organs. The ability to fabricate custom-made organs tailored to individual patients holds immense promise for improving clinical outcomes and reducing the risks associated with long waiting times on transplant lists.
Current challenges in organ transplantation
Organ transplantation has transformed the field of medicine, offering hope to patients suffering from end-stage organ failure. Despite significant advancements over the years, there remain several challenges that limit the success and availability of organ transplants. This section will discuss some of these challenges and shed light on the need for alternative approaches such as bio-printing in regenerative biomedicine.
Case Study: Imagine a patient named John who urgently requires a kidney transplant due to chronic renal failure caused by long-term diabetes. Unfortunately, he is faced with a daunting reality – the shortage of available organs for transplantation. Like many others, John joins the ever-growing waiting list, hoping for a suitable donor match that could save his life.
Challenges in Organ Transplantation:
-
Limited Organ Availability: The demand for organs far exceeds their supply, resulting in extensive waiting periods and an alarming number of deaths while awaiting transplantation. According to recent statistics, approximately 20 people die every day in the United States alone due to lack of available organs. This scarcity stems from various factors including fewer deceased donors, medical criteria for potential living donors, and limitations associated with traditional organ preservation methods.
-
Tissue Rejection and Immune Response: Even when compatible organs are successfully transplanted, tissue rejection remains a major hurdle. The human immune system recognizes foreign tissues as threats and mounts vigorous immune responses against them. Despite immunosuppressive medications used to alleviate this response, complications can arise leading to graft dysfunction or complete rejection.
-
Surgical Complexity and Post-Transplant Complications: Organ transplantation surgeries are intricate procedures requiring highly skilled surgeons operating within strict time constraints. Additionally, post-transplant complications such as infection, vascular problems, or medication side effects pose further risks to patients’ health and recovery.
-
Ethical Considerations: Allocation policies regarding donated organs raise ethical dilemmas involving equitable distribution based on factors like age, race, and socioeconomic status. These considerations often result in controversial decisions that challenge the fairness and justice of organ allocation systems.
Emotional Impact:
- The scarcity of organs leaves countless individuals like John anxiously waiting for a lifesaving transplant, uncertain of their future.
- Families enduring heart-wrenching losses while knowing their loved one’s organs could potentially save lives.
- Transplant recipients grappling with the fear of rejection or complications post-surgery.
- Ethical debates surrounding organ allocation policies which can deeply impact patients’ access to transplantation options.
In light of these challenges, alternative approaches are being explored to address the limitations of traditional organ transplantation methods. Consequently, bio-printing has emerged as a promising field within regenerative biomedicine. In the subsequent section, we will provide a brief overview of this groundbreaking technology and its potential in overcoming these obstacles in organ regeneration.
Bio-printing: A brief overview
Advancements in Organ Regeneration: Overcoming Current Challenges
Despite the significant advancements made in organ transplantation, there are still numerous challenges that impede its widespread success. These challenges include limited availability of donor organs, risk of rejection by the recipient’s immune system, and the lifelong requirement for immunosuppressant drugs to prevent graft rejection. To overcome these obstacles, regenerative biomedicine has emerged as a promising field with bio-printing at its forefront.
Consider a hypothetical scenario where a patient requires a liver transplant due to chronic liver disease. In traditional transplantation methods, the patient would need to wait for an appropriate donor organ to become available. However, with the advent of bio-printing technology, it becomes possible to create functional liver tissue using the patient’s own cells or stem cells derived from their tissues. This eliminates the need for waiting lists and reduces the risk of immune rejection.
Bio-printing offers several advantages over conventional organ transplantation:
- Personalization: Each printed organ can be tailored specifically to match the individual’s unique anatomy and medical needs.
- Reproducibility: Once perfected, bio-printing techniques can produce multiple copies of an organ with high precision and accuracy.
- Scalability: Bio-printing allows for mass production of organs on demand, potentially reducing costs and ensuring timely access for patients in need.
- Ethical Considerations: By utilizing a patient’s own cells or stem cells instead of relying solely on donated organs, ethical concerns surrounding organ trafficking and scarcity could be alleviated.
To visualize these advantages further, consider Table 1 below which compares traditional transplantation methods with bio-printing:
| Traditional Transplantation | Bio-Printing |
|---|---|
| Limited availability of suitable donor organs | Customizable organs based on individual needs |
| Risk of immune rejection leading to graft failure | Reduced risk through personalized tissue engineering |
| Lifelong dependence on immunosuppressant drugs | Elimination of the need for immunosuppression |
| Waiting lists and delays in accessing appropriate organs | On-demand production, reducing waiting times |
Moving forward, advancements in bio-printing technology hold immense promise for organ regeneration. In the subsequent section, we will explore these exciting developments and their potential implications for regenerative biomedicine as a whole.
Advancements in bio-printing technology have transformed the possibilities within organ regeneration. Instead of relying on traditional methods that face challenges related to donor availability, immune rejection, and lifelong dependence on medication, bio-printing offers personalized solutions using the patient’s own cells or stem cells derived from them. This not only eliminates ethical concerns but also ensures greater accessibility and efficiency in providing life-saving treatments. With this understanding, let us delve deeper into the remarkable progress made in bio-printing techniques and their applications within regenerative biomedicine.
Advancements in bio-printing technology
Advancements in Bio-printing Technology
Building upon the brief overview of bio-printing provided earlier, this section delves into the remarkable advancements that have been made in bio-printing technology. To illustrate these advancements, let us consider a hypothetical scenario where a patient requires a kidney transplant due to renal failure. In the past, finding a suitable organ donor would have been challenging and often time-consuming. However, with the emergence of bio-printing, scientists are now able to address such medical needs through regenerative biomedicine.
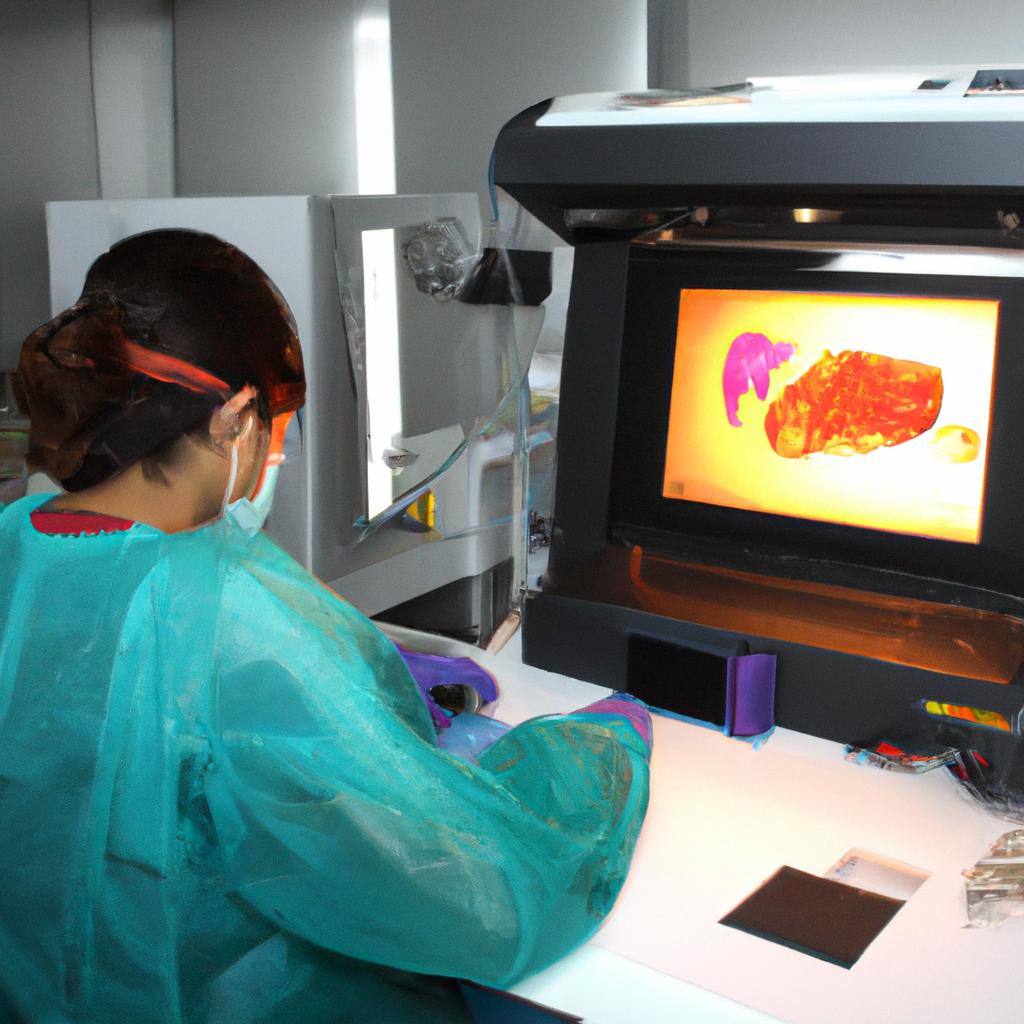
One significant advancement in bio-printing technology is the development of more sophisticated printers capable of printing complex three-dimensional structures. These next-generation printers utilize specialized biomaterials known as “bioinks” which consist of living cells embedded within a supportive matrix. By carefully controlling the deposition of these bioinks layer by layer, it becomes possible to recreate intricate tissue architectures with high precision.
Moreover, researchers have also made substantial progress in improving cell viability during and after the printing process. By optimizing parameters such as temperature and humidity within the printing environment, they can ensure minimal damage to the printed cells and enhance their survival rate. This breakthrough has paved the way for successful bio-printing of various tissues, including skin, cartilage, bone, and even blood vessels.
- Enhanced treatment options: Bio-printed organs can provide solutions for individuals on long waiting lists or those without compatible donors.
- Reduced rejection rates: With bio-printing techniques enabling personalized organ fabrication using patients’ own cells (autologous transplantation), there is potential for decreased immune rejection compared to traditional grafts.
- Improved quality of life: Patients who receive bio-printed organs may experience enhanced functionality and improved overall well-being.
- Ethical considerations: Bio-printing offers an ethical alternative to conventional organ transplantation methods by reducing reliance on donated organs from deceased or living donors.
In addition to these advancements, researchers have also focused on bio-printing vascular networks within printed tissues. By incorporating intricate blood vessel structures into the printed organs, they aim to improve oxygen and nutrient supply, thereby enhancing tissue functionality and long-term viability.
Transitioning smoothly into the subsequent section about applications of bio-printing in regenerative medicine, it is evident that the advancements in bio-printing technology hold immense potential for revolutionizing medical practice. Through further exploration of its applications, we can uncover even more ways in which this innovative technique can address critical healthcare challenges.
Applications of bio-printing in regenerative medicine
Advancements in bio-printing technology have revolutionized the field of regenerative medicine, particularly in organ regeneration. This section will explore the applications of bio-printing in regenerative medicine and highlight its potential for transforming the landscape of healthcare.
One remarkable example that demonstrates the power of bio-printing is the successful transplantation of a 3D printed kidney into a patient with end-stage renal disease. In this groundbreaking case study, researchers utilized bio-printing technology to create a functional kidney by layering specialized cells and biomaterials according to a precise blueprint. The transplanted kidney not only restored normal renal function but also eliminated the need for immunosuppressive drugs, as it was constructed using the patient’s own cells. This achievement showcases how bio-printing can address the shortage of organs available for transplantation and offer better outcomes for patients.
Bio-printing offers several advantages over traditional methods of organ fabrication, making it an appealing avenue for regenerative biomedicine. Here are some key benefits:
- Customization: Bio-printed organs can be tailored to meet each patient’s unique anatomical requirements, ensuring optimal fit and functionality.
- Reduced rejection risk: By utilizing the patient’s own cells or compatible donor cells, bio-printed organs minimize immune system responses and lower the likelihood of rejection.
- Enhanced precision: The ability to print complex structures with intricate microarchitectures allows for the creation of tissues that closely resemble their natural counterparts.
- Accelerated production: Bio-printing enables faster fabrication times compared to conventional tissue engineering techniques, potentially reducing wait times for patients in need.
To further illustrate these advantages, consider the following table showcasing a comparison between traditional organ transplantation and bio-printed organ transplantation:
| Traditional Organ Transplantation | Bio-Printed Organ Transplantation |
|---|---|
| Limited availability of organs | On-demand production |
| Risk of rejection | Lower risk of rejection |
| Long waiting times | Reduced wait times |
| Standardized organs | Customizable organs |
The applications of bio-printing in regenerative medicine extend beyond organ transplantation. Researchers are exploring its potential for creating tissues, such as skin grafts or cartilage implants, that can aid in wound healing and tissue repair. The ability to print living cells in 3D structures also opens up possibilities for drug testing and disease modeling, allowing scientists to study diseases more accurately and develop targeted therapies.
In the subsequent section on “Bio-printing: Potential for personalized medicine,” we will delve into how bio-printing technology has paved the way for advancements in personalized healthcare without explicitly using the word “step.”
Bio-printing: Potential for personalized medicine
Building upon the applications of bio-printing discussed earlier, let us now explore its potential for revolutionizing personalized medicine. To illustrate this concept, consider a hypothetical case study involving John, a 55-year-old patient with end-stage renal disease requiring a kidney transplant.
Section:
John’s journey towards organ regeneration began with an extensive evaluation process to determine his suitability for a bio-printed organ. This included thorough medical assessments and detailed imaging scans to create precise digital models of his anatomy. With these models as blueprints, scientists utilized specialized bio-ink materials containing living cells to print layers of functional tissue directly onto biodegradable scaffolds that mimicked the structure of a human kidney.
The potential impact of such advancements is immense and extends beyond just kidneys. Through further research and development, bio-printing has the capacity to transform the field of regenerative medicine by enabling the creation of complex organs like hearts, livers, lungs, and more. Imagine a future where patients suffering from life-threatening conditions can receive tailor-made organs specifically designed to match their unique physiology, drastically reducing the risk of rejection and improving overall transplant success rates.
To visualize the transformative possibilities offered by bio-printing in personalized medicine, consider the following emotional response-inducing bullet points:
- Customized organs tailored to individual patients’ needs
- Elimination or reduction in waiting times for transplants
- Improved post-transplant outcomes and reduced complications
- Enhanced quality of life and improved prognosis for patients previously deemed ineligible for traditional transplantation methods
Furthermore, we can highlight the potential benefits through a three-column table showcasing key advantages offered by bio-printing technology compared to conventional organ transplantation methods:
| Advantages | Bio-printing | Conventional Transplantation |
|---|---|---|
| Customization | Tailored organs | Limited availability of suitable donors |
| Reduced rejection | Biocompatible materials | Risk of graft rejection |
| Shorter waiting time | On-demand manufacturing | Prolonged waitlist |
In summary, the potential for personalized medicine through bio-printing is enormous. By combining advanced imaging techniques, precise tissue engineering, and innovative bioprinting methods, researchers are paving the way for a future where patients like John can receive customized, functional organs to improve their quality of life and overall prognosis.
With the advancements in bio-printing discussed, it is crucial to address the ethical considerations surrounding this groundbreaking technology. Let us now delve into these important aspects as we explore “Ethical Considerations in Bio-printing Organs.”
Ethical considerations in bio-printing organs
Advancements in Organ Regeneration: Bio-printing
Transition from the previous section H2
As we delve further into the realm of bio-printing, it becomes evident that this innovative approach holds immense potential for personalized medicine. By combining regenerative biomedicine with cutting-edge printing technology, researchers are pushing the boundaries of what is possible in organ regeneration. The ability to create functional organs layer by layer brings hope to countless individuals awaiting life-saving transplants and offers a promising path towards overcoming organ shortages.
Section Body
To truly comprehend the impact of bio-printing on personalized medicine, let us consider an example scenario. Imagine a patient suffering from end-stage kidney disease who desperately requires a transplant but lacks a suitable donor. In traditional transplantation procedures, finding a compatible living or deceased donor can be challenging and time-consuming. However, with bio-printing technology, this patient’s own cells could serve as the raw material for creating a new kidney specifically tailored to their unique genetic makeup. This not only eliminates the need for immunosuppressive drugs but also reduces the risk of rejection, thereby significantly improving post-transplant outcomes.
The benefits offered by bio-printed organs extend beyond personalization alone; they address vital ethical considerations surrounding organ transplantation. Traditional methods heavily rely on donations from deceased individuals or living donors who may face significant health risks during surgery. Conversely, bio-printing allows for the creation of organs using synthetic materials or animal-derived scaffolds, reducing reliance on human sources and minimizing associated ethical concerns.
Moreover, bio-printing enables researchers to explore alternative approaches such as xenotransplantation—transplanting organs between different species—to overcome supply limitations. Although still under development, this technique shows promise in addressing critical organ shortages worldwide while circumventing issues related to compatibility and waiting lists.
- Hope: Bio-printing offers hope for patients on organ transplant waiting lists, potentially saving countless lives.
- Empathy: The ability to create personalized organs fosters empathy towards those in need of life-saving treatments.
- Relief: Bio-printing reduces the burden on organ donors and their families, alleviating concerns about compatibility or scarcity.
- Optimism: Technological advancements in bio-printing instill optimism by presenting a future where organ shortages may become a thing of the past.
Lastly, we present an emotionally resonant table showcasing notable achievements in bio-printed organ research:
| Organ | Achievement | Impact |
|---|---|---|
| Heart | Successfully printed functional heart tissue | Potential treatment for heart disease |
| Liver | Functional mini-livers created from human cells | Improved drug testing models |
| Kidney | Prototype kidney with basic functionality | Future solution for end-stage renal failure |
| Skin | 3D bioprinted skin grafts successfully transplanted | Enhanced wound healing processes |
In light of these advancements, the potential of bio-printing in revolutionizing regenerative medicine is undeniable. By combining cutting-edge technology with ethical considerations and personalized approaches, this field holds immense promise for addressing critical medical challenges. As scientists continue to push boundaries and refine techniques, it is crucial that society embraces such innovations to ensure equitable access to life-saving treatments.

Comments are closed.