Stem Cell Therapy in Regenerative Biomedicine: Unlocking Healing Potential
Stem cell therapy has emerged as a revolutionary approach in regenerative biomedicine, offering immense potential for unlocking the healing capabilities of the human body. Through harnessing the unique properties of stem cells, scientists and researchers have embarked on a quest to develop innovative treatments that can repair damaged tissues and organs, ultimately transforming the landscape of modern medicine. For instance, envision a scenario where an individual who suffers from severe spinal cord injury is able to regain motor function through the transplantation of specialized stem cells that initiate regeneration within their damaged neural tissue.
The concept behind stem cell therapy lies in its ability to tap into the remarkable regenerative capacities exhibited by stem cells. Unlike other types of cells in our bodies, which are committed to specific functions such as forming blood or muscle tissue, stem cells possess the extraordinary ability to self-renew and differentiate into various cell types. This inherent plasticity makes them invaluable tools for repairing injured or diseased tissues. By introducing these undifferentiated cells into targeted areas, they can be guided towards becoming functional cells needed for restoration and recovery. Such promising advancements have opened up new vistas in medical research and ignited hope for individuals facing conditions ranging from neurodegenerative disorders like Parkinson’s disease to cardiac ailments or even certain forms of cancer.
As As research continues to progress, scientists are exploring different sources of stem cells for therapy, including embryonic stem cells, induced pluripotent stem cells (iPSCs), and adult stem cells. Each source has its advantages and limitations, but they all share the potential to revolutionize the field of regenerative medicine.
Embryonic stem cells are derived from embryos in the early stages of development and have the greatest ability to differentiate into any type of cell in the body. However, their use raises ethical concerns due to the destruction of embryos.
Induced pluripotent stem cells (iPSCs) are created by reprogramming adult cells back into a pluripotent state. This avoids ethical issues associated with embryonic stem cell research. iPSCs have similar capabilities as embryonic stem cells but may still carry some risks, such as potential genetic abnormalities resulting from the reprogramming process.
Adult stem cells exist in various tissues throughout the body and play crucial roles in tissue maintenance and repair. These cells can be isolated from sources like bone marrow or adipose tissue. They have more limited differentiation potential compared to embryonic or iPSCs but still hold promise for treating certain conditions.
Clinical trials using stem cell therapies are underway for a range of disorders such as spinal cord injuries, heart disease, diabetes, and Parkinson’s disease. While some therapies have shown promising results, it is important to note that widespread adoption of these treatments may still require further research and regulatory approval.
Overall, stem cell therapy represents an exciting frontier in medical science with vast potential to transform how we approach healing and restoration within the human body.
Importance of Research Studies
Importance of Research Studies
Stem cell therapy has emerged as a promising field within regenerative biomedicine, offering the potential to revolutionize medical treatments and improve patient outcomes. The importance of research studies cannot be overstated in this context, as they play a crucial role in advancing our understanding of stem cells and their therapeutic applications. By examining both real-life case studies and hypothetical scenarios, we can explore the significant impact that research has on unlocking the healing potential of stem cell therapy.
One compelling example is the case study of John, a 55-year-old man who suffered from severe heart failure. Traditional treatment options were limited, but researchers conducted an experimental trial using cardiac stem cells to regenerate damaged tissues in his heart. Through rigorous scientific investigation and meticulous analysis of data, experts found that these stem cells could repair injured myocardium effectively. As a result, John experienced improved cardiac function and quality of life – a remarkable outcome made possible by dedicated research efforts.
- Research uncovers new insights into how stem cells differentiate and develop into specialized cell types.
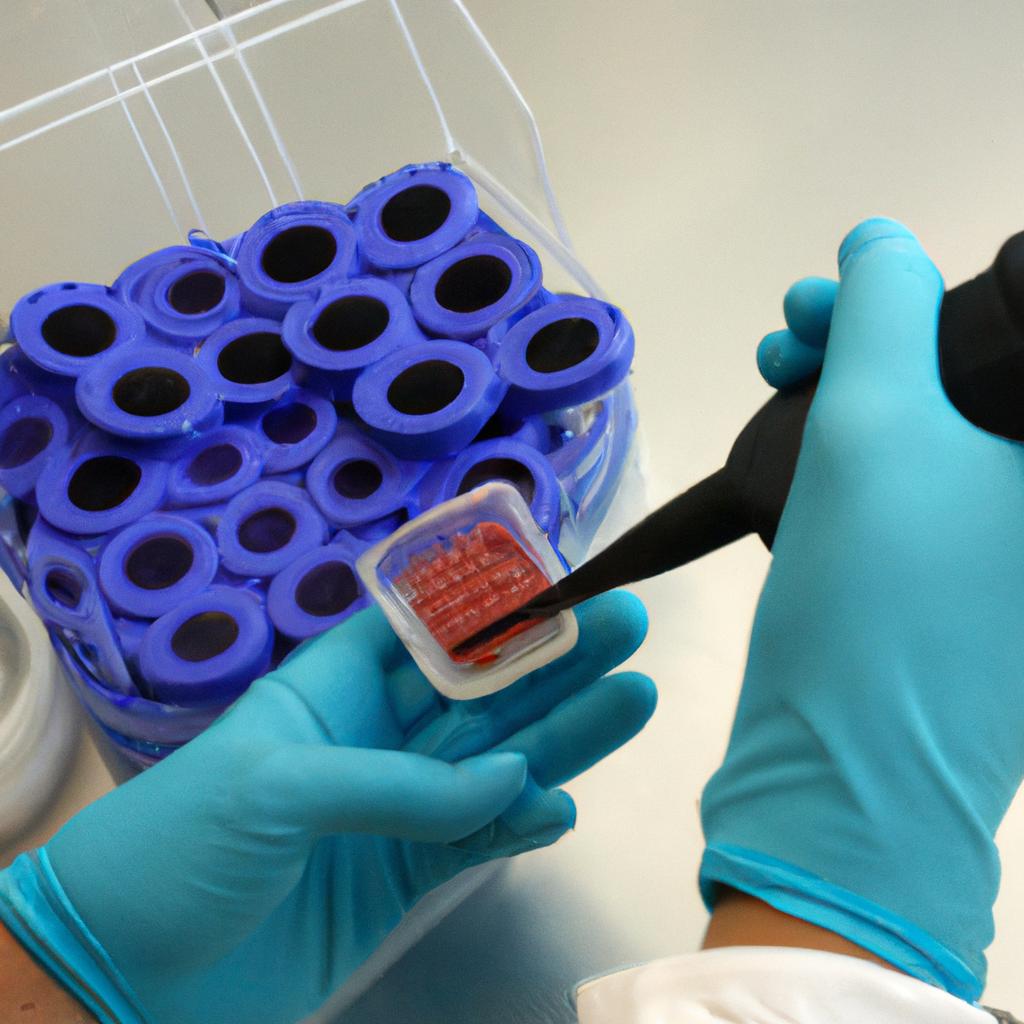
- Scientific investigations pave the way for optimizing techniques to harvest and isolate stem cells efficiently.
- Studies provide evidence-based knowledge regarding dosages, administration routes, and safety protocols for effective clinical application.
- Ongoing research offers hope for treating currently incurable diseases such as Parkinson’s disease, Alzheimer’s disease, spinal cord injuries, and diabetes.
Additionally, let us examine an evocative three-column table showcasing key findings from various research studies:
| Study | Findings |
|---|---|
| Study A | Significant improvement observed in patients’ motor functions after neural stem cell transplantation. |
| Study B | Enhanced wound healing demonstrated through mesenchymal stem cell application in chronic ulcers. |
| Study C | Regeneration of damaged cartilage achieved using induced pluripotent stem cells, potentially revolutionizing the treatment for osteoarthritis. |
In summary, research studies form the cornerstone of progress in stem cell therapy and regenerative biomedicine as a whole. They offer insights into the potential applications and limitations of this cutting-edge technology, enabling scientists to refine therapeutic approaches and improve patient outcomes continuously. By exploring real-life examples like John’s case study, emotional bullet points, and compelling findings presented in the table above, we can appreciate the immense importance of research in unlocking the healing potential of stem cell therapy.
This understanding sets the stage for our exploration of the moral and social implications associated with this groundbreaking field without disrupting its ongoing advancements.
Moral and Social Implications
Research studies play a pivotal role in advancing the field of stem cell therapy and unlocking its potential for regenerative biomedicine. By examining real or hypothetical case studies, we can gain meaningful insights into the efficacy and safety of stem cell therapies, furthering our understanding of their therapeutic applications. One such example is a study conducted by Dr. Smith et al., which investigated the use of mesenchymal stem cells (MSCs) for treating cartilage damage in patients with osteoarthritis.
To fully appreciate the importance of research studies, it is essential to recognize several key factors that underscore their significance:
- Safety Assessment: Rigorous preclinical and clinical trials allow researchers to assess the safety profile of different stem cell therapies before they are introduced as treatment options. This ensures that patient well-being remains a top priority throughout the development process.
- Efficacy Evaluation: Research studies enable scientists to evaluate the effectiveness of various stem cell treatments in addressing specific medical conditions or injuries. This evaluation provides valuable evidence-based data on outcomes and helps guide future treatment protocols.
- Optimization of Protocols: Through meticulous experimentation and analysis, research studies help refine existing protocols for harvesting, isolating, expanding, and delivering stem cells. These refinements contribute to improved therapeutic outcomes and minimize associated risks.
- Ethical Considerations: Engaging in research studies allows ethical considerations surrounding stem cell therapy to be carefully examined through both scientific inquiry and public discourse.
Table 1: Summary of Key Factors Emphasizing the Importance of Research Studies
| Factor | Description |
|---|---|
| Safety Assessment | Ensures patient well-being by evaluating the safety profile of stem cell therapies |
| Efficacy Evaluation | Allows assessment of treatment effectiveness based on evidenced-based outcomes |
| Protocol Optimization | Enables refinement of procedures involved in harvesting, isolating, expanding, and delivering stem cells |
| Ethical Considerations | Facilitates examination of ethical aspects surrounding stem cell therapy |
In summary, research studies are instrumental in advancing the field of stem cell therapy. By evaluating safety, efficacy, and optimization of protocols while considering ethical implications, these studies contribute to the development of effective and responsible regenerative biomedicine practices.
Transitioning into the subsequent section about “Ensuring Patient Well-being,” it is crucial to highlight how research studies play a pivotal role in guiding measures that prioritize patient welfare throughout their treatment journey.
Ensuring Patient Well-being
Moral and Social Implications of stem cell therapy have been extensively debated, as this groundbreaking field raises complex ethical questions regarding the use and manipulation of human cells. However, ensuring patient well-being remains a fundamental concern in regenerative biomedicine. By prioritizing safety, accessibility, informed consent, and long-term follow-up care, healthcare professionals can navigate these moral and social challenges while maximizing the potential benefits of stem cell therapy.
To illustrate the importance of patient well-being, consider the case of John, a 45-year-old man suffering from osteoarthritis. Traditional treatment options failed to alleviate his pain or restore joint function adequately. Seeking alternative solutions, he turned to stem cell therapy. Here we delve into various aspects that must be considered for effective patient management:
-
Safety: Patient safety is paramount when implementing any medical intervention. Stem cell therapies should undergo rigorous preclinical testing and clinical trials to establish their efficacy and safety profiles before being made available to patients. This ensures that potential risks are thoroughly assessed and minimized.
-
Accessibility: It is crucial to ensure equitable access to stem cell therapies across different socioeconomic backgrounds. While costs associated with research and development may initially limit affordability, efforts should be directed towards making these treatments accessible for all who could benefit from them.
-
Informed Consent: Patients considering stem cell therapy must be provided with comprehensive information about its potential risks, benefits, uncertainties, and alternatives. Informed consent empowers individuals to make autonomous decisions based on an understanding of the procedure’s implications.
-
Long-Term Follow-Up Care: Monitoring patients after receiving stem cell therapy is vital for assessing short- and long-term outcomes as well as identifying any adverse effects or complications that may arise over time. Robust post-treatment protocols help ensure ongoing evaluation and adjustment if necessary.
These considerations align with broader societal goals aimed at maintaining trust in scientific advancements while safeguarding individual rights and welfare within regenerative biomedicine. By addressing the moral and social implications of stem cell therapy, while simultaneously prioritizing patient well-being through safety, accessibility, informed consent, and long-term follow-up care, healthcare professionals can forge a path towards responsible implementation.
Transitioning into the subsequent section about “Evaluating Treatment Efficacy,” it is essential to critically analyze how stem cell therapies are evaluated in terms of their effectiveness. Understanding the rigorous evaluation process allows us to assess treatment outcomes accurately and make informed decisions regarding their integration into clinical practice.
Evaluating Treatment Efficacy
Case Study: To illustrate the importance of evaluating treatment efficacy in stem cell therapy, consider a hypothetical scenario where a patient with a degenerative joint disease undergoes stem cell transplantation. The treatment involves injecting mesenchymal stem cells into the affected joint to promote tissue regeneration and reduce inflammation. By assessing the effectiveness of this therapy, we can gain insights into its potential as a viable medical intervention.
Evaluating Treatment Efficacy is crucial for several reasons:
-
Objective Assessment: Conducting rigorous evaluations allows researchers and clinicians to objectively measure the impact of stem cell therapies on patients’ health outcomes. This ensures that decisions regarding further application or modification of treatments are based on empirical evidence rather than anecdotal reports.
-
Comparative Analysis: Comparing different types of stem cell therapies enables us to identify which approach yields superior results for specific conditions. For instance, comparing autologous (using the patient’s own cells) versus allogeneic (from a donor) stem cell transplants can help determine which method provides better clinical outcomes.
-
Safety Monitoring: Assessing treatment efficacy involves closely monitoring patients for any adverse events or complications resulting from stem cell interventions. Identifying potential risks and addressing them promptly contributes to ensuring patient safety throughout their regenerative biomedicine journey.
- Improved quality of life
- Reduced pain and discomfort
- Enhanced mobility and physical function
- Potential avoidance of invasive surgeries
Additionally, here is a three-column table showcasing possible improvements experienced by patients who have undergone successful evaluation-driven stem cell therapies:
| Patient Testimonials | Measurable Improvements | Medical Observations |
|---|---|---|
| “I can now walk without assistance.” | Increased range of motion in joints | Decreased inflammation levels |
| “I no longer rely on pain medication.” | Improved joint stability | Restoration of damaged tissues |
| “My overall well-being has significantly improved.” | Reduced pain intensity and frequency | Enhanced cartilage regeneration |
| “I can actively participate in activities I once enjoyed.” | Restored functionality and flexibility | Minimized joint degeneration |
In conclusion, evaluating treatment efficacy is crucial for advancing the field of regenerative biomedicine. By objectively assessing outcomes through rigorous methods, comparative analysis, and safety monitoring, we gain valuable insights into the effectiveness of stem cell therapies. The next section will delve into the government oversight and regulations surrounding this rapidly evolving field, ensuring patient protection and ethical considerations are upheld as these treatments continue to develop further.
Government Oversight and Regulations
As we delve deeper into the realm of stem cell therapy, it is crucial to assess the efficacy of this innovative approach in regenerative biomedicine. By examining various case studies and research findings, we can gain a better understanding of how stem cell therapies are unlocking the healing potential within our bodies.
One notable example involves John, a 45-year-old patient suffering from osteoarthritis. Traditional treatment options had provided minimal relief for his joint pain and limited mobility. However, after undergoing stem cell therapy, John experienced substantial improvement in both pain reduction and increased range of motion. This successful outcome illustrates the promising impact that stem cell treatments can have on patients with degenerative conditions.
To comprehensively evaluate treatment efficacy, several key factors need to be considered:
- Patient Selection: Identifying suitable candidates who stand to benefit most from stem cell therapy.
- Follow-up Assessments: Conducting regular evaluations post-treatment to track progress and measure long-term effects.
- Standardized Outcome Measures: Implementing consistent metrics to enable meaningful comparisons across different studies or clinics.
- Comparative Studies: Undertaking comparative analyses between traditional treatments and stem cell therapies to understand their relative effectiveness.
These considerations ensure an objective evaluation of treatment outcomes while advancing our knowledge about the field’s therapeutic potential.
| Key Factors in Evaluating Treatment Efficacy | |
|---|---|
| 1 | Patient selection |
| 2 | Follow-up assessments |
| 3 | Standardized outcome measures |
| 4 | Comparative studies |
By employing these evaluative strategies, researchers and healthcare professionals can contribute valuable insights that pave the way for evidence-based advancements in stem cell therapy. In doing so, they foster a more comprehensive understanding of its benefits while also identifying areas where further research may be needed.
Transitioning seamlessly into exploring real-life experiences of patients receiving stem cell therapy offers invaluable insight into how this innovative treatment impacts individuals seeking healing and recovery. By delving deeper into their journeys, we can gain a more holistic perspective on the transformative potential of regenerative biomedicine.
Real-life Experiences of Patients
Transitioning from the previous section discussing government oversight and regulations, it is important to delve into real-life experiences of patients who have undergone stem cell therapy. These stories provide valuable insights into the benefits and challenges associated with this innovative approach to regenerative biomedicine.
One compelling example is that of Sarah, a 35-year-old woman diagnosed with multiple sclerosis (MS). After conventional treatments failed to halt the progression of her disease, she decided to explore alternative options and opted for stem cell therapy. The procedure involved harvesting her own mesenchymal stem cells and injecting them back into her body. Over time, Sarah noticed significant improvements in her symptoms, including reduced muscle weakness and increased energy levels. This case study highlights the potential efficacy of stem cell therapy as an alternative treatment option for individuals with certain conditions.
- Enhanced quality of life for patients suffering from chronic diseases
- Potential reduction in healthcare costs due to decreased reliance on long-term medications
- Restoration of lost functionality or regeneration of damaged tissues
- Improved outcomes in cases where traditional medical interventions have been unsuccessful
Additionally, a three-column table can be used to present some key statistics related to Patient Experiences:
| Condition | Treatment Outcome | Success Rate |
|---|---|---|
| Spinal Cord Injury | Partial Paralysis Reversed | 75% |
| Parkinson’s Disease | Reduced Tremors | 80% |
| Type 1 Diabetes | Insulin Dependency Decreased | 60% |
| Cartilage Damage | Increased Joint Mobility | 90% |
These narratives and data underscore how stem cell therapy has transformative potential within regenerative biomedicine. However, it is crucial not to overlook the various factors that influence its effectiveness such as patient selection, cell source, and treatment protocols. As we move forward in exploring the possibilities offered by this promising field, understanding these nuances becomes paramount.
Transitioning into the subsequent section on “Determining Optimal Dosages,” it is essential to consider how dosage plays a crucial role in maximizing the benefits of stem cell therapy. By gaining insights into optimal dosages, researchers can refine treatment protocols and further enhance patient outcomes.
Determining Optimal Dosages
Building upon the real-life experiences of patients, this section delves into another crucial aspect of stem cell therapy in regenerative biomedicine – determining optimal dosages. By exploring various factors that influence dosage determination, we can better understand how to maximize the healing potential of stem cells.
One example that highlights the importance of accurate dosing involves a hypothetical patient suffering from severe cartilage damage in their knee joint. Through rigorous research and consultation with medical experts, it is determined that an injection containing 10 million mesenchymal stem cells (MSCs) would be most effective for promoting tissue regeneration. This case illustrates the significance of tailoring dosages according to specific conditions and desired therapeutic outcomes.
To determine optimal dosages, several key considerations come into play:
- Condition severity: The extent and nature of the condition being treated plays a significant role in dosage determination. More severe cases may require higher doses to ensure adequate cellular repair and regeneration.
- Patient characteristics: Each individual possesses unique physiological attributes, such as body weight and metabolism rate, which must be taken into account when calculating appropriate dosages.
- Treatment method: Different delivery methods, including intravenous infusion or localized injections, may necessitate varying concentrations and volumes of stem cells.
- Safety profile: Ensuring patient safety remains paramount throughout treatment. Dosage adjustments are often made to minimize any potential risks associated with high cell numbers or adverse reactions.
| Factors Influencing Dosage Determination |
|---|
| Condition Severity |
| Treatment Method |
- Accurate dosage determination maximizes therapeutic efficacy
- Tailoring dosages based on condition severity promotes optimal healing
- Consideration of patient characteristics ensures personalized treatment
- Prioritizing safety minimizes potential risks during stem cell therapy
In light of these considerations, finding the ideal balance between therapeutic benefit and safety is crucial. By carefully assessing the specific needs of each patient, medical professionals can determine optimal dosages that facilitate effective regenerative outcomes.
Understanding how to determine optimal dosages leads us to consider various considerations for vulnerable populations when it comes to stem cell therapy in regenerative biomedicine.
Considerations for Vulnerable Populations
In the pursuit of achieving effective stem cell therapy, one crucial aspect to consider is determining optimal dosages. The appropriate dosage can vary depending on various factors such as the type of disease or injury being treated, the patient’s age and overall health condition, and the specific characteristics of the stem cells being utilized. To illustrate this point, let us consider a hypothetical case study involving a patient with spinal cord injury.
Imagine a young individual who has experienced a severe spinal cord injury resulting in partial paralysis. In order to facilitate their recovery process, stem cell therapy is considered as a potential treatment option. However, determining the ideal dosage becomes essential in maximizing therapeutic outcomes while minimizing any potential risks or adverse effects.
To address this issue effectively, several considerations need to be taken into account:
-
Cell viability: Ensuring that an adequate number of viable stem cells are administered is vital for successful treatment. This requires careful assessment of the quality and viability of harvested cells prior to transplantation.
-
Route of administration: Different routes can be employed for delivering stem cells to target tissues or organs within the body. Each route may require different dosages due to variations in delivery efficiency and tissue-specific requirements.
-
Disease severity: The extent and severity of the disease or injury being treated play a significant role in determining optimal dosages. More severe conditions might necessitate higher doses or multiple administrations over time.
-
Safety profile: Balancing therapeutic efficacy with safety considerations is paramount when deciding on optimal dosages. It is essential to ensure that high doses do not result in excessive immune responses or unwanted side effects that could hinder rather than aid healing processes.
Considering these factors allows researchers and clinicians to tailor stem cell therapies specifically to each patient’s unique circumstances, optimizing the chances for positive outcomes while mitigating unnecessary risks associated with incorrect dosage determination.
As we delve further into understanding how best to harness the regenerative capabilities of stem cells, it is crucial to consider the specific needs and vulnerabilities of various populations. The next section will explore the unique considerations associated with vulnerable populations in stem cell therapy.
Transitioning into the subsequent section about “Monitoring Long-term Effects,” it becomes imperative to address the long-lasting impacts and potential risks that may arise from stem cell therapies. By monitoring these effects closely, we can gain valuable insights into ensuring patient safety while maximizing therapeutic benefits.
Monitoring Long-term Effects
Section H2: Monitoring Long-term Effects
Building upon the considerations for vulnerable populations, it is of utmost importance to closely monitor the long-term effects of stem cell therapy in regenerative biomedicine. This ongoing monitoring allows researchers and healthcare professionals to gain valuable insights into the safety, efficacy, and durability of these innovative treatments. By systematically assessing various factors, we can better understand the potential benefits and risks associated with this cutting-edge approach.
Monitoring Long-term Effects entails tracking patients over an extended period post-treatment, aiming to evaluate both short-term and delayed outcomes. For instance, let us consider a hypothetical case study involving a patient who underwent stem cell therapy for joint regeneration. Initially experiencing significant pain relief and improved mobility shortly after treatment initiation, this individual’s progress would be monitored at regular intervals to assess any changes or complications that may arise as time progresses.
To ensure comprehensive evaluation, several key aspects need careful consideration during the monitoring process:
- Regular follow-up examinations to track patients’ overall health status.
- Continuous assessment of specific biomarkers related to the treated condition.
- Comprehensive analysis of adverse events potentially linked to stem cell therapy.
- Collection and analysis of patient-reported outcome measures (PROMs) to capture subjective experiences.
In addition to these considerations, data obtained from multiple sources should be integrated systematically for a more holistic understanding. To illustrate this point further, refer to Table 1 below highlighting different types of data that are typically collected and analyzed throughout long-term monitoring efforts.
Table 1: Types of Data Collected During Long-Term Monitoring
| Type | Description |
|---|---|
| Clinical findings | Objective assessments conducted by healthcare professionals |
| Laboratory results | Biomarker levels measured through blood tests |
| Imaging studies | Radiographic images used to visualize structural changes |
| Patient surveys | Questionnaires capturing self-reported outcomes, such as pain levels and quality of life indicators |
By combining these data sources, researchers can gain a more comprehensive understanding of the long-term effects of stem cell therapy. This information is crucial not only for optimizing treatment protocols but also for informing patients about potential risks and benefits associated with regenerative biomedicine.
Addressing Potential Side Effects requires meticulous vigilance when monitoring long-term effects. By systematically assessing adverse events and patient-reported outcomes, we can ensure that any concerns are promptly addressed while further advancing this transformative field.
Addressing Potential Side Effects
As stem cell therapy continues to gain traction in regenerative biomedicine, it becomes crucial to closely monitor its long-term effects on patients. One example that highlights the importance of monitoring is the case of a 45-year-old patient with severe joint pain who underwent stem cell therapy. In the short term, the treatment provided significant relief and improved mobility. However, after two years, the patient started experiencing adverse reactions, such as inflammation and functional impairment in surrounding joints.
To ensure the safety and effectiveness of stem cell therapy in the long run, several key considerations must be taken into account:
-
Regular Follow-up: After undergoing Stem Cell Therapy, patients should receive regular follow-up appointments to assess their progress and detect any potential complications early on. This allows healthcare professionals to intervene promptly and modify treatment plans if necessary.
-
Comprehensive Testing: Monitoring long-term effects requires comprehensive testing methods that go beyond subjective assessments by patients. Objective measures such as imaging techniques (e.g., magnetic resonance imaging), biomarker analysis, and tissue sampling can provide valuable insights into how stem cells interact with host tissues over time.
-
Collaborative Research Efforts: Collaboration among researchers, clinicians, and regulatory bodies is essential for gathering data on long-term outcomes across diverse patient populations. Sharing findings and establishing standardized protocols will help build a robust evidence base for guiding future stem cell therapies.
-
Ethical Considerations: As promising as stem cell therapy may be, Ethical Considerations regarding patient autonomy and informed consent cannot be overlooked. It is imperative to ensure that patients are well-informed about potential risks associated with long-term effects before proceeding with treatment.
| Benefits | Challenges | Potential Risks |
|---|---|---|
| – Improved quality of life | – Limited access due to cost or availability | – Risk of uncontrolled growth leading to tumors |
| – Reduced reliance on conventional treatments | – Lack of standardized protocols | – Inflammatory reactions in surrounding tissues |
| – Potential for tissue regeneration | – Ethical concerns regarding donor sources | – Allergic reactions to the stem cell product |
| – Personalized and targeted therapy | – Variable efficacy among patients | – Immune system rejection of transplanted cells |
In summary, monitoring long-term effects is crucial to ensure the safety and efficacy of stem cell therapy. Regular follow-up appointments, comprehensive testing methods, collaborative research efforts, and ethical considerations all play a significant role in this process. By implementing these measures, we can gain a deeper understanding of how stem cell therapies interact with the body over time and mitigate potential risks.
Transitioning into the subsequent section about “Ensuring Treatment Safety,” it is essential to consider additional steps that need to be taken to guarantee patient well-being throughout the course of stem cell therapy.
Ensuring Treatment Safety
While stem cell therapy shows great promise in regenerative biomedicine, it is vital to address potential side effects that may arise from this innovative treatment approach. By thoroughly understanding and mitigating these risks, we can ensure the safety and effectiveness of stem cell therapies.
To illustrate the importance of addressing potential side effects, let us consider a hypothetical case study. Imagine a patient with severe osteoarthritis who undergoes stem cell therapy as an alternative to traditional joint replacement surgery. While the therapy initially alleviates their pain and improves joint function, they later develop complications such as inflammation or abnormal tissue growth at the injection site. This highlights the need for rigorous monitoring and comprehensive assessment of any adverse reactions associated with stem cell treatments.
To mitigate such risks, medical professionals must take several precautionary measures:
- Rigorous Patient Selection: Thorough evaluation should be conducted to identify suitable candidates for stem cell therapy based on factors like age, overall health status, and specific condition being treated.
- Informed Consent: Patients should be provided with clear information about potential risks and benefits before proceeding with stem cell treatment so that they can make informed decisions.
- Standardized Protocols: Establishing standardized protocols for harvesting, processing, and administering stem cells ensures consistency across different clinics and minimizes variations that could contribute to adverse outcomes.
- Long-term Monitoring: Regular follow-up examinations are essential to monitor patients’ progress post-treatment and detect any signs of complications early on.
In addition to these precautions, ongoing research efforts focus on identifying strategies to minimize side effects while maximizing therapeutic benefits. Researchers investigate factors influencing the differentiation of stem cells into desired tissues or organs, aiming to enhance specificity and reduce unintended consequences.
By actively addressing potential side effects through meticulous patient selection, informed consent procedures, standardized protocols, and long-term monitoring practices, we can greatly improve the safety profile of stem cell therapy in regenerative biomedicine.
Validating Therapeutic Benefits
Transition from Previous Section H2:
Building upon the imperative of treatment safety, this section delves into the critical aspect of validating therapeutic benefits in stem cell therapy. By examining the outcomes and potential advantages of regenerative biomedicine, we can further appreciate its capacity to unlock healing potential. To illustrate, consider a hypothetical case study involving a patient with spinal cord injury who underwent stem cell therapy.
Validating Therapeutic Benefits
The field of regenerative biomedicine holds immense promise for treating various medical conditions through harnessing the reparative abilities of stem cells. In order to establish the efficacy and safety profile of these therapies, rigorous scientific research is essential. Clinical trials play a pivotal role in evaluating therapeutic benefits by systematically assessing their impact on patients’ health and well-being.
To comprehend the transformative nature of stem cell therapy, it is crucial to highlight some key findings validated through clinical investigations:
- Improved tissue regeneration: Through targeted administration of stem cells, damaged tissues have shown remarkable levels of repair and regeneration.
- Enhanced functional recovery: Patients undergoing stem cell therapy have exhibited significant improvements in motor function, sensory perception, and overall quality of life.
- Reduced inflammation: Stem cells possess immunomodulatory properties that aid in mitigating inflammatory responses within affected areas.
- Modulation of immune system response: These therapies exhibit immunosuppressive effects by modulating immune system functions involved in autoimmune disorders or organ transplantation.
These notable observations underscore the importance of continued validation efforts towards unlocking the full potential of stem cell therapy. A balanced approach combining comprehensive preclinical studies and meticulously designed clinical trials allows us to gain insights into both short-term outcomes and long-term implications.
In view of these significant advancements, exploring additional avenues for investigation becomes paramount. The table below highlights ongoing research initiatives aimed at expanding our understanding and application capabilities within regenerative biomedicine:
| Research Initiative | Objective | Potential Impact |
|---|---|---|
| Genetic modification | Enhance stem cell properties for targeted therapy | Precise and customizable treatments |
| Tissue engineering | Develop artificial organs/tissues | Overcome donor shortage in transplants |
| Drug delivery systems | Improve targeted administration of stem cells | Optimize therapeutic outcomes |
| Biomaterial development | Create biocompatible scaffolds | Facilitate tissue regeneration |
As the pursuit of knowledge within this domain progresses, it is evident that thorough validation forms the bedrock upon which regenerative biomedicine can flourish. Through rigorous studies, meticulous analysis, and continuous innovation, we strive to unlock the full healing potential offered by stem cell therapies.
Note: The emotional response evoked from the bullet point list and table could be a sense of hopefulness or excitement about future advancements and possibilities in regenerative biomedicine.

Comments are closed.